|
|
Head: Prof. Vladimír Holáň, PhD, DScE-mail: holan@biomed.cas.cz |
The department is primarily focused on the study of cellular and molecular mechanisms specific to transplantation immunity and to use this knowledge in the regulation of immune responses. The aim is to improve the survival of genetically diverse cells and tissue transplants.
The basic model proposed involves the use of cultured and specifically differentiated stem cells (mesenchymal, limbic), which are transplanted with different kinds of nanofiber media for the purpose of repairing severe damage to the skin and ocular surface as well as replenishing limbal stem cell deficiencies. It uses a wide range of methods of cell and molecular biology, such as cell cultures, differentiation of stem cells, the study of gene regulation (PCR, real time PCR), the production and detection of cytokines using assays(ELISA, ELISPOT), flow cytometry, MACS, Western blotting, experimental models of transplantation of skin, cornea, limbus, and stem cell transfers.Themain objective is to test the knowledge gained in preclinical models and their potential use in clinical practice (particularly in patients with severe ocular surface wounds).
|
Research Scientists: Prof. Vladimír Holáň, PhD, DSc
PhD Students:
Undergraduate Students: Pavla Boháčová Jan Kössl
Technicans: |
Research topics
The transplantation of an organ or the transfer of stem cells often represents the only way to improve or even to rescue the life of a patient. However, immunological rejection represents a major obstacle to the further development of therapeutic transplantation. Therefore, deep knowledge of the molecular and cellular mechanisms of the transplantation reaction is required. Using a model of immunological reaction to histocompatibility antigens, we have focused our research on studying the activation and function of regulatory T cells in transplantation immunity and tolerance. Using a model of orthotopic corneal and limbal transplantation, we have analyzed the details of ocular immunity. Since successful treatment of the severely damaged ocular surface requires the transfer of limbal stem cells, we recently started to isolate, grow and characterize stem cells. We succeeded in isolating limbal and mesenchymal stem cells in the mouse and using them for the repair of the damaged corneal epithelium. For the transfer of stem cells, we use various types of nanofibre scaffolds, which represent optimal 3D matrices for stem cell growth. Well-established methods for monitoring the immune response enabled us, in co-operation with other laboratories, to study the cytokine response in various experimental models of immunoregulation. The ultimate goal of our research is to acquire insights into the mechanisms of the specific immune response, to isolate and transplant stem cells and to propose novel strategies for targeted immunoregulation.
Recent experiments have also been focused on the targeted differentiation of mesenchymal stem cells in vitro and their use for ocular surface reconstruction. This is one of our models for testing the possibilities of using stem cell transplantation in regenerative and reparative medicine.
|
Fig. 1: Experimental model of skin grafting in inbred strains of mice. Skin allografts in mice are protected by bandages for 10 days, then the survival of the grafts in immunomodulated recipients is monitored and evaluated.
|
|
Fig. 2: The scheme of the regulatory role of cytokines in the development of individual phenotypically and functionally distinct subpopulations of T lymphocytes.
|
|
Fig. 3: Flow cytometry analysis of the in vitro induction and development of regulatory T lymphocytes and proinflammatory Th17 cells. Spleen cells from BALB/c mice were cultured with irradiated cells from B6 mice in the absence or presence of the determining cytokines TGF-ß and IL-6, and the percentage of regulatory T cells (Foxp3+ cells) or Th17 cells (RORγt+ cells) was determined by FACS analysis.
|
|
Fig. 4: Expression of genes for immunologically relevant molecules in rejected corneal allografts and xenografts in an experimental mouse model. Corneal grafts were transplanted orthotopically, and the expression of genes for the tested molecules was detected in individual corneas by PCR. Lanes 1,2 – healthy cornea, 3,4 – corneal autografts, 5.6 – corneal allografts, 7,8 – corneal xenografts.
|
Important results in 2013
1. Regeneration of severely damaged ocular surface by stem cells
Limbal and mesenchymal stem cells were cultured in vitro on nanofiber scaffolds and transferred on the damaged ocular surface in experimental animal models. The therapeutic effects of stem cells were evaluated by histology and according to the ability to inhibit expresssion of genes for proinflammatory molecules IL-2, IFN-gama, IL-17 and iNOS. The results thus demonstrate the ability of stem cells and nanofiber scaffolds to regenerate ocular surface after the injury.
Collaboration: Evropská oční klinika Lexum, Praha.
|
|
A scheme of immunoregulatory and therapeutic effects of mesenchymal stem cells. There are number of diferent mechanisms by which MSC contribute to the healing process. Differentiation into epithelial-like cells, immunomodulation and the production of growth and trophic factors are the most important mechanisms. |
|
A structure of nanofiber scaffold (A) and the growth of mesenchymal stem cells on nanofiber scaffold (B, C). (A) Scanning electron microscopy image of nanofibers from copolymer polyamid 6/12, the avarage nanofiber diameter is 380 nm, (B) Mouse MSC growing on nanofibers (red filaments – F-actin stained with phalloidin, blue – DAPI staining of the nuclei), (C) Scanning electron microscopy of mouse MSC growing on nanofibers.
|
|
|
Chemically damaged eye of the rabbit covered by a nanofiber scaffold with stem cells. The application of a nanofiber scaffold seeded with MSC onto the damaged ocular surface of a rabbit.
|
Publications:
- Holáň, V., Javorková, E.: (2013) Mesenchymal stem cells, nanofiber scaffolds and ocular surface reconstruction. Stem Cells Rev. Rep. 9(5), 609-619. IF 4.523
- Čejková J., Tošan P., Čejka Č., Lenčová A., Zajícová A., Javorková E., Kubinová Š., Syková E., Holáň V.: (2013) Suppression of alkali-induced oxidative injury to the cornea by mesenchymal stem cells growing on nanofiber scaffolds and transferred onto the damaged corneal surface. Exp. Eye Res. 116, 312-323. IF 3.026
- Holáň, V., Javorková, E., Trošan, P.: The growth and delivery of mesenchymal and limbal stem cells using copolymer polyamide 6/12 nanofiber scaffolds. In: Wright, B. and Connon, C. J. (eds), Corneal Regenerative Medicine, Methods Mol. Biol., Humana Press – Springer, New York, London 2013, S. 187-199. ISBN 978-1-62703-431-9.
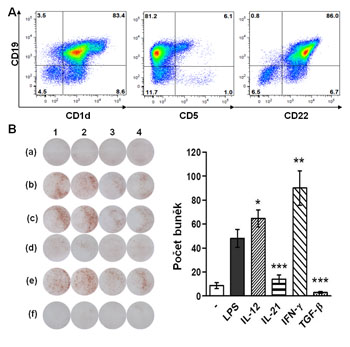
2. Distinct roles of cytokines in the development of regulatory T cells and regulatory B cells
The role of cytokines in development of regulatory T (Treg) and B (Breg) cells was described. TGF-beta was shown as the main cytokine determining the development of Tregs, but this cytokine inhbited activation of IL-10-producing Breg. On the contrary, another two cytokines, IL-12 and IFN-gama, enhanced the development of Breg. These results show distinct roles of cytokines in development of Treg and Breg, and suggest new approaches for targeted regulation of the immune system.
Collaboration: Přírodovědecká fakulta UK, Praha
|
|
(A) Characterization of B cell populations by flow cytometry. (B) Detection of cells producing IL-10 using technology ELISPOT.
|
Publications:
- Holáň, V., Zajícová, A., Javorková, E., Trošan, P., Chudičková, M., Pavlíková, M., Krulová, M.: (2013) Distinct cytokines balance the development of regulatory T cells and IL-10-producing regulatory B cells. Immunology. In press. IF 3.705
- Kubera M., Curzytek K., Duda W., Leskiewicz M., Basta-Kaim A., Budziszewska B., Roman A., Zajícová A., Holáň V., Szczesny E., Lason W., Maes M.:. (2013) A new animal model of (chronic) depression induced by repeated and intermittent lipopolysaccharide administration for 4 months. Brain Behav. Immun. 31, 96-104. IF 5.612
- Holáň, V., Krulová, M.: (2013) Common and small molecules as the ultimate regulatory and effector mediators of antigen-specific transplantation reactions. World J. Transplant. 3(4), 54-61. (nový časopis, zatím bez IF)
Laboratory of Eye Histochemistry and Pharmacology
Laboratory of Histochemistry and Pharmacology eye examines the causes of non-healing lesions anterior eye segment in various eye injury or illness and regeneration of tissues anterior segment of the eye, particularly the cornea, with the restoration of visual function. For the healing of anterior eye segment lesions, special attention is paid to the nanofibers as carriers of stem cells and dosage forms.
Assoc. Prof. Jitka Čejková, MD, DSc | Head of Laboratory
E-mail: cejkova@biomed.cas.cz
Phone: +420 241 062 208
Research Scientists:
Assoc. Prof. Jitka Čejková, MD, DSc
Čestmír Čejka, MSc, PhD
Laboratory technician:
Jana Herlova
Pre-graduated students:
Tomanová Aneta
Vašková Věrča
Švandová Ivana
Bayerová Martina
|
Spectrophotometry results of the corneal center, expressed either as the spectrum of transmittance T = T (λ) (A) or absorbance A = A (λ) (B). The spectral curves are means from measurements of 14 normal corneas, 7 irradiated with UVA rays (1. 1 J/cm2, once a day for 5 days), 6 irradiated with a double dose of UVA (2. 2 J/cm2, once a day for 5 days), and 7 irradiated with UVB (1. 1 J/cm2, once a day for 5 days). Note that for wavelengths shorter than about 300 nm, the spectra show the instrumental stray light error rather than the corneal optical properties. The corneas repeatedly irradiated with UVB rays (daily dose of 1. 01 J/cm2 for five days) absorb more light throughout the whole measurable spectral range than do normal corneas. In contrast, no significant differences between normal corneas and corneas irradiated with UVA rays (daily dose of 1. 01 J/cm2 or a double dose, for five days) were found (tested at 320, 380, and 550 nm by one-way ANOVA with Dunnett´s post-test).
|
|
Immunohistochemical staining of pro-inflammatory cytokines
(IL 1-β, IL-6, IL-8, THF-α) in the human conjunctival epithelium of autoimmune dry eye disease (Sjögren´s syndrome, SS). Scale bar: 10 μM. The severity of pro-inflammatory cytokine expression parallels the severity of the symptoms of dryness and the slit-lamp findings. Normal conjunctival cytology samples revealed no or very weak cytokine staining (mature interleukin-1beta (IL 1-β), Fig. 1 a; interleukin 6 (IL-6), Fig. 1 d; interleukin 8 (IL-8), Fig. 1 g; tumor necrosis factor alpha (TNF-α), Fig. 1 j). Only nuclei were stained with haematoxylin. However, all cytokines studied were already expressed in the conjunctival epithelium of dry eye (SS) grade 2, moderate symptoms of dryness with reversible slit-lamp findings (IL 1-β, Fig. 1 b; IL-6, Fig. 1 e; IL-8, Fig. 1 h; TNF-α Fig. 1 k), and their expression increased in the conjunctival epithelium of dry eye (SS) grade 3, severe symptoms of dryness with irreversible slit lamp findings (IL 1-β Fig. 1 c; IL-6, Fig. 1 f; IL-8, Fig. 1 i; TNF-α, Fig. 1 l). Arrows point to cytokine expression. |
Important results in 2013
1. New regenerating agent (RGTA, CACICOL 20) for the healing of chronic corneal injuries and diseases
We proved that new regenerating agent (RGTA, CACICOL20) is effective for the healing of corneal injuries, particularly of poorly healing chronic ulcers. Following RGTA topical application the expression of proteolytic enzymes (mainly metalloproteinases) and enzymes that generate nitric oxide gradually decreased, accompanied by the positive corneal healing without scarring. Corneal neovascularization and inflammation were reduced. Corneal transparency recovered totally or at least partially.
|
Representative photographs of rabbit eyes with ulcers developed after the injury of the cornea with 1.0 N NaOH and subsequently treated with RGTA or placebo.
a - The control eye; b - The cornea of the first eye one day after the injury with 1.0 N NaOH. Corneal transparency is lost; c - The cornea of the first eye after one month following the injury (the cornea without any treatment). Corneal ulcer develops (black arrow); d - The cornea of the first eye after subsequent treatment with RGTA for one month. The ulcer is healed (black arrow); e – The cornea of the second eye one day after the injury with 1.0 N NaOH. The corneal transparency is lost. f – The cornea of the second eye after one month – for this time interval the cornea was without any treatment. The central corneal ulcer develops (arrow). g – The cornea of the second eye after four weeks of subsequent placebo treatment. The ulcer is developed (black arrow) and highly persisted (h). The cornea is vascularized.
|
|
Expression of genes for proinflammatory cytokines in alkali-injured corneas from placebo- and RTGA-treated eyes.
Corneas from the eyes injured by alkali and treated with placebo or RGTA were harvest on day 7 (after 0.15 N NaOH) (A) or day 21 (after 1.0 N NaOH) (B) and the expression of genes for IL-1beta (a), IFN- (b) and iNOS (c) were determined by real-time PCR. Each bar represents the mean +-S.D. from at least 3 determinations. Values with asterisks are significantly (*P<0.05, ***P<0.01) different from placebo treated corneas. |
Collaboration: Thea Laboratoires, Clermont Ferrand, France (Dr.Celine Olmiere), Department of Transplantation Immunology, (prof. RNDr Vladimír Holáň, DrSc.)
Publication: Cejkova J, Olmiere C, Cejka C, Trosan P, Holan V (2013). The healing of alkali-injured cornea is stimulated by a novel matrix regenerating agent (RGTA, CACICOL20): a biopolymer mimicking heparan sulfates reducing proteolytic, oxidative and nitrosative damage. Histol Histopathol 2013 Oct 9. (29,457-78,2014).IF 2,281.
2. Rabbit mesenchymal stem cells growing on nanofiber scaffolds heal oxidative injury of the cornea evoked by alkali burns
Rabbit mesenchymal stem cells growing on nanofiber scaffolds and transferred onto the damaged corneal surface healed oxidative injury of the cornea evoked by alkali. Alkali injury evoked the imbalance between corneal oxidants and antioxidants leading to the increased expression of pro-inflammatory cytokines, and to the formation of nitrotyrosine and malondialdehyde. Mesenchymal stem cells significantly reduced corneal oxidative stress and healed the cornea with the restoration of transparency.
|
Representative photograps of alkali-injured corneas (with 0.15 N NaOH) (A-G), corneal neovascularization (H) and vascular endothelial growth factor (VEGF) (I) on day 15 after the injury.
A - healthy eye; B - immediately after the injury the cornea turs grayish; C - injured cornea on which nanofiber scaffolds with mesenchymal stem cells (MSCs) were transferred and sutured with conjunctiva; D, E - In alkali-injured cornea untreated with MSCs high neovascularization (grade 4) (D) or middle neovascularization (grade 3) (E) appeared. E, F - In contrast, in alkali injured cornea treated with MSCs only low neovascularization developed (grade 2) (F) or only solely vessels could be found (grade 1) (G). H - Quantification of corneal neovascularization by counting vessels. I – Quantification of corneal neovascularization using real-time PCR (the expression of genes for VEGF).
|
|
Haematoxylin-eosin staining (HE) (a,b), expression of Vascular endothelial factor (VFGF) (C-F) and expression of macrophages (g-j) on day 15 after the injury of the cornea with 0.15 N NaOH.
a – In the injured untreated cornea numerous inflammatory cells are present in the vascularized stroma (arrows); b – In contrast, the injured cornea treated with MSCs is without vessels and the number of inflammatory cells is highly reduced; c, e – In untreated injured cornea VEGF expression is highly pronounced, whereas in injured cornea treated with MSCs VEGF expression is low, nearly as in the control cornea (f). In untreated injured cornea high number of macrophages is seen (g, i). In contrast, in injured cornea treated with MSCs only solely macrophages can be found (h); j – Control cornea, macrophages are not present. |
Collaboration: Department of Neuroscience (prof. MUDr Eva Syková, DrSc.), Department of Transplantation Immunology (prof. RNDr Vladimír Holáň, DrSc.)
Publication: Cejkova J, Trosan P, Cejka C, Lencova A, Zajicova A, Javorkova E, Kubinova S, Sykova E, Holan V (2013). Suppression of alkali-induced oxidative injury in the cornea by mesenchymal stem cells growing on nanofiber scaffolds and transferred onto the damaged corneal surface. Exp Eye Res 116:312-323.IF 3,026.